Moving Past Disbelief in Systemic Racism to Understand What it Means For Health Equity
March 23, 2021
Overview
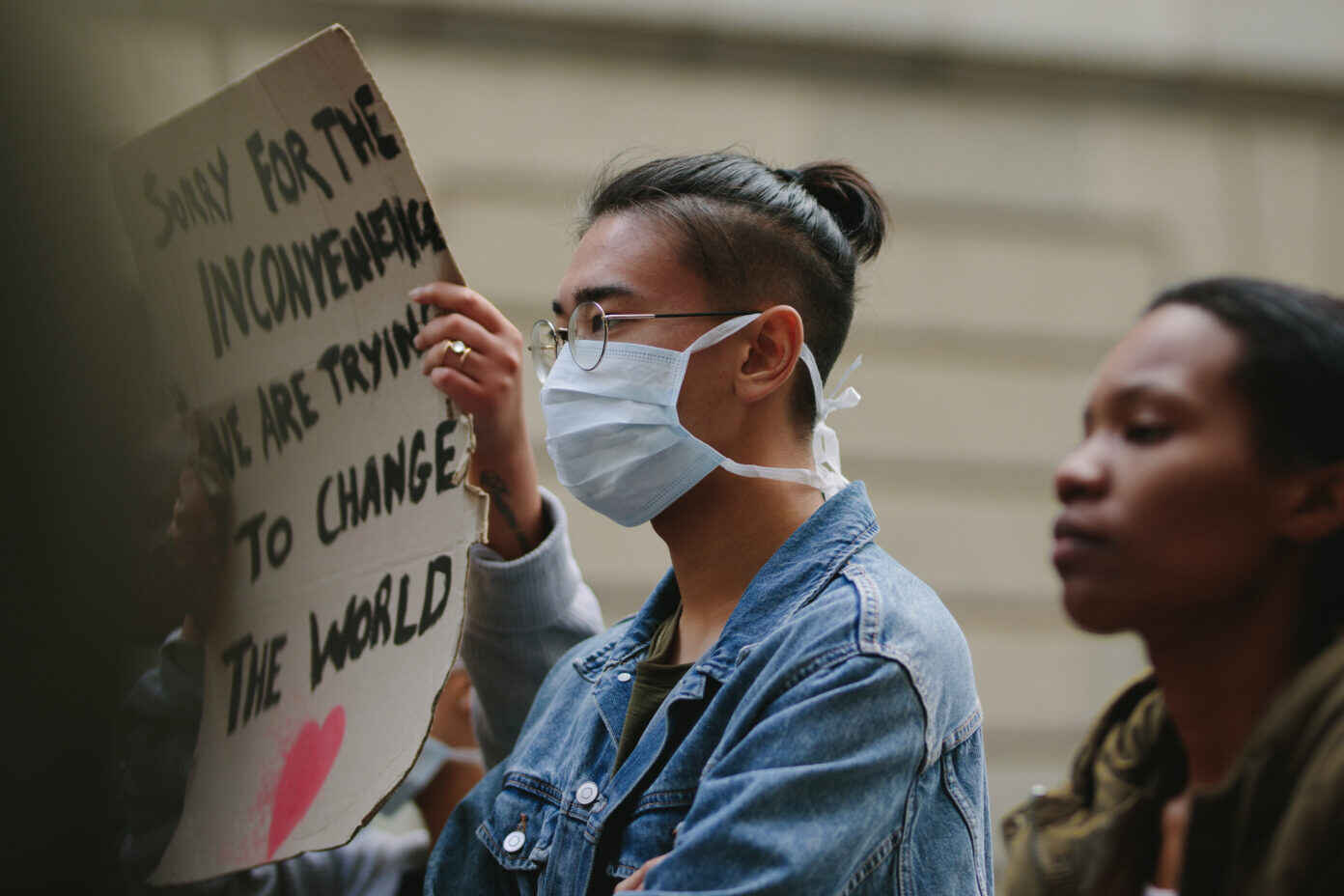
Since the Biden Administration released its plan to advance racial equity in the United States, there has been significant pushback against the idea that systemic racism even exists. This questioning is not new, but it has taken on a renewed fervor as state and local governments, professional associations, hospitals and health systems, and corporations have made public commitments to addressing systemic racism and treating racism as a public health crisis.
In the past month, we have seen Sen. Tom Cotton question newly confirmed Attorney General Merrick Garland about whether President Biden’s racial equity orders are themselves racist or discriminatory. We have seen Students for Fair Admissions file a petition asking the Supreme Court to overturn a 2003 ruling that allows the limited use of race and ethnicity in college admissions. And we have seen the Journal of the American Medical Association release a podcast on social media with the caption: “No physician is racist, so how can there be structural racism in health care?”
What is structural or systemic racism? It is the differences in access to power, resources, and opportunity by race that are codified and normalized in laws, policies, practices, and institutions, including the government. Simply put, it is a system that ensures that people of color are at a disadvantage, and it is so engrained in our society that it is perpetuated and reinforced regardless of intention. What does it mean to treat racism as a public health crisis? As Dr. Sandro Galea has described, it means that the problem “must affect large numbers of people, it must threaten health over the long-term, and it must require the adoption of large-scale solutions.”
Some examples of the effects of systemic racism across different systems and sectors include:
- In government: the systematic denial of FHA loans in the 1930s and 1940s to people of color both for purchasing new homes and for upgrading existing homes, a policy (known as redlining) that was backed by the U.S. government and reinforced by racial restrictive covenants in property deeds. This is directly connected to racial disparities in homeownership today.
- In institutions: the American Medical Association commissioning a report in the early 1900s that led to the closure of Black medical schools that can be linked to a shortage of at least 27,000 Black physicians through 2019. In just one example of why this matters, a recent study of Florida births found that Black newborn babies are more likely to survive when cared for by Black doctors than when cared for by white doctors.
- In Medicaid: the segregation of nursing homes by race due to historical Medicaid policy and the lack of Medicaid expansion in states where 60 percent of uninsured adults are people of color, despite evidence that Medicaid expansion has reduced disparities in health care access and coverage.
- In the legal system: the exclusion of people of color from serving on juries whether due to implicit bias or purposeful discrimination, and it is the disproportionate incarceration of Black, Latinx, and American Indian youth in the juvenile justice system, caused in part by harsher punishment of youth of color. This problem isn’t limited to youth. One study in Florida found that Black people are more likely to be found guilty, receive longer sentences, and have fewer opportunities to undergo alternative sentencing options rather than spending time in jail or prison. Mass incarceration affects health by leading to a higher prevalence of chronic health conditions and lower life expectancy post-release.
- In corporations: meat and poultry plants failing to adequately protect workers – who are disproportionately people of color and immigrants – from COVID-19. This, combined with inadequate enforcement of workplace safety laws and punitive attendance policies, among other issues, led to 87 percent of reported cases of COVID-19 at these plants occurring among racial and ethnic minority workers.
- In advertising: the intentional marketing of tobacco products and sugary drinks to communities of color, ultimately leading to higher rates of lung disease and other chronic conditions like diabetes.
The effects of systemic racism have also been painfully evident during the COVID-19 pandemic. Black, Latinx, and American Indian people are experiencing more cases, hospitalizations, and deaths due to COVID-19 relative to their share of the population, not because of personal choices, but because of social and structural conditions that create greater risks for some communities than others. Lack of homeownership leads to people of color being concentrated in more crowded communities or living in more crowded housing with intergenerational families (limiting the ability to isolate and increasing the risk for elders). Due to the history of redlining, these communities are often located near environmental hazards that increase risk for conditions like asthma and COPD; risk factors for COVID-19.
People of color are disproportionately represented in essential worker positions, have less access to health insurance and primary care (partially thanks to Medicaid policies), and may lack social supports like childcare, paid sick leave, paid time off, and other workplace protections. People of color are also inadequately represented in law and medicine, on corporate boards, and in leadership positions across industries. What all this means is that people of color are more vulnerable to COVID-19 but have fewer resources to deal with the risk and fewer people in positions of power who call attention to the problem and help do something about it.
Systemic racism is a problem that affects large groups of people, threatens health over the long term, and requires large-scale solutions. Yet in an ongoing survey about health, equity, and race amid COVID-19, 22.1 percent of respondents strongly disagree that systemic racism is a reason for poorer health outcomes among people of color, and another 10.8 percent somewhat disagree. The evidence is there, but too many people do not understand it or fail to see the connection. We have to do a better job of communicating that racial equity doesn’t mean that white people will be disadvantaged if people of color stop being disadvantaged, as though it’s a requirement in this country that some group of people has to be disadvantaged. Looking at systems through a racial equity lens means recognizing that no group of people has to be disadvantaged to benefit another group of people. Social justice benefits all of us, and the time to act is now.
Here are five things that public health professionals, leaders, and partners can do:
- Assess your own biases (we all have them to some degree) and educate yourself on the history of your community (start with maps of redlined communities in your state at Mapping Inequality).
- Be a better community member. Volunteer, diversify the news you read and the media you access, support minority-owned businesses, and be intentional about assessing and expanding your network to include people from different backgrounds and with different experiences.
- Step up your civic participation. Contact state and local leaders about issues that matter to you and your community. Demand accountability for commitments that your leaders make. And vote in all elections to ensure that we have officials at every level of government who understand the interests and needs of the communities they serve.
- Assume that we all value the same things. Even if we don’t all show our values in the same way, this is a good starting point to find common ground in talking about issues that you care about in your community.
- If you’re comfortable talking about systemic racism and its effects – keep doing it. Not every conversation has to be exactly perfect, they never are. But we have to begin somewhere. We can only normalize these kinds of conversations by having them.
This post was written by Dawn Hunter, Deputy Director, Network for Public Health Law – Southeastern Region Office.
The Network for Public Health Law provides information and technical assistance on issues related to public health. The legal information and assistance provided in this post do not constitute legal advice or legal representation. For legal advice, readers should consult a lawyer in their state.
Support for the Network is provided by the Robert Wood Johnson Foundation (RWJF). The views expressed in this post do not represent the views of (and should not be attributed to) RWJF.
